Diabetes Emergency Plan: What You Must Know to Stay Safe
Navigating life with diabetes requires constant vigilance. It is a condition that demands careful management. Unexpected events can quickly escalate into serious health crises. A well-defined diabetes emergency plan is not merely a suggestion; it is a necessity. This plan acts as a crucial lifeline. It provides guidance during times of stress and uncertainty. It ensures prompt and appropriate action. This article provides essential information. It will help you create a comprehensive diabetes emergency plan. This plan will protect your health and well-being.
Understanding Diabetes Emergencies
Diabetes, a metabolic disorder, affects how your body processes sugar (glucose). This sugar comes from the food you eat. Without proper treatment, diabetes can lead to dangerous complications. These complications can quickly become life-threatening. Recognizing the signs of these emergencies is the first step. It allows for immediate and effective intervention. The most common diabetes emergencies include:
- Hypoglycemia (Low Blood Sugar): This occurs when blood glucose levels drop too low.
- Hyperglycemia (High Blood Sugar): This happens when blood glucose levels rise too high.
- Diabetic Ketoacidosis (DKA): This is a severe complication of diabetes. It is most common in people with type 1 diabetes.
- Hyperosmolar Hyperglycemic State (HHS): This is a serious complication. It is most common in people with type 2 diabetes.
Each of these emergencies presents unique symptoms and risks. They require immediate medical attention.
Recognizing the Symptoms
Early detection is critical in managing diabetes emergencies. Understanding the symptoms is paramount. This allows you to respond quickly and effectively. Here’s what to look for:
Hypoglycemia
Low blood sugar can develop rapidly. It can cause a range of symptoms. These include:
- Shaking
- Sweating
- Anxiety
- Dizziness
- Rapid heartbeat
- Confusion
- Blurred vision
- Seizures
- Loss of consciousness
If you experience these symptoms, check your blood glucose immediately. Treat with fast-acting carbohydrates. [See also: Managing Hypoglycemia in Everyday Life]
Hyperglycemia
High blood sugar develops more gradually. It can present with the following symptoms:
- Increased thirst
- Frequent urination
- Blurred vision
- Fatigue
- Headache
- Nausea and vomiting
- Abdominal pain
- Shortness of breath
- Fruity-smelling breath (DKA)
If you experience these symptoms, check your blood glucose. Contact your healthcare provider for guidance.
Creating Your Diabetes Emergency Plan
A well-crafted diabetes emergency plan should be personalized. It needs to reflect your specific needs and circumstances. It should include the following key components:
Medical Information
This section should contain essential medical details. This is vital for first responders and healthcare providers. Include:
- Your name and date of birth
- Contact information for your primary care physician and endocrinologist
- A list of all your medications, including dosages and times
- Information about any allergies
- Your type of diabetes (type 1 or type 2)
- Any other relevant medical conditions
Keep this information readily accessible. Carry a medical ID card or wear a medical alert bracelet. This is crucial in an emergency.
Emergency Contacts
List the names and contact information of your emergency contacts. These can be family members, friends, or caregivers. Ensure they are aware of your diabetes emergency plan. Make sure they know how to respond in an emergency.
Blood Glucose Monitoring
Regular blood glucose monitoring is essential. Include instructions on how to check your blood sugar levels. This must be done during an emergency. Specify the target blood glucose range. Also, include instructions on how to use your blood glucose meter. Make sure to include the steps for checking ketones if needed.
Treatment for Hypoglycemia
Develop a clear plan for treating low blood sugar. This plan should include:
- Instructions on how to administer fast-acting carbohydrates.
- The amount of glucose tablets or other carbohydrates to use.
- Guidelines on when to recheck blood glucose levels.
- Instructions on when to seek medical attention.
- Information on how to administer glucagon if prescribed.
Treatment for Hyperglycemia
Outline steps to manage high blood sugar. This should include:
- Instructions on how to administer insulin, if prescribed.
- Guidance on when to check for ketones.
- Instructions on when to contact your healthcare provider.
- Information on when to seek immediate medical care.
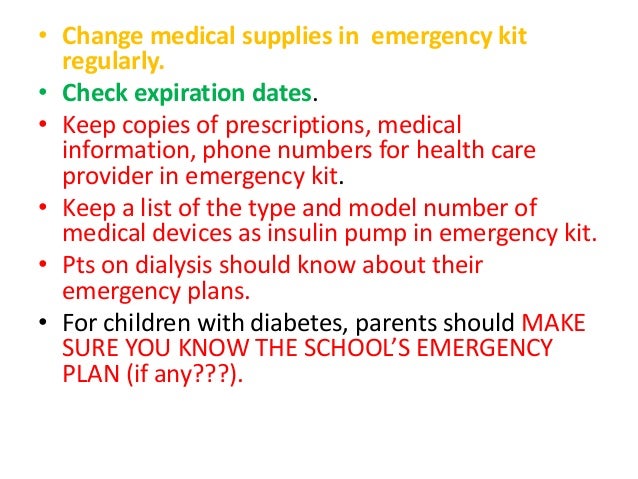
Emergency Medications and Supplies
Gather all necessary medications and supplies. Keep them in a designated emergency kit. This kit should include:
- Insulin (if prescribed) and syringes or insulin pens
- Glucagon emergency kit
- Blood glucose meter and test strips
- Ketone test strips
- Fast-acting carbohydrates (glucose tablets, juice, etc.)
- Medical ID card or bracelet
- Contact information for your healthcare providers
- A copy of your diabetes emergency plan
Ensure your emergency kit is easily accessible. Regularly check the expiration dates of your medications. Replace any expired items.
Educating Your Support Network
Share your diabetes emergency plan with your support network. This includes family, friends, and colleagues. Ensure they understand your condition and the steps to take. This is in case of an emergency. Conduct regular training sessions. These sessions should cover the following:
- Recognizing the symptoms of hypoglycemia and hyperglycemia
- Knowing how to administer glucagon (if applicable)
- Understanding how to contact emergency services
- Knowing where to find your emergency kit
Educating your support network is crucial. It ensures everyone can act swiftly and effectively. This is during a diabetes emergency.
When to Seek Immediate Medical Attention
Certain situations require immediate medical attention. These include:
- Loss of consciousness or confusion
- Seizures
- Severe abdominal pain
- Difficulty breathing
- Vomiting
- Fruity-smelling breath
- Blood glucose levels consistently above 300 mg/dL or below 70 mg/dL despite treatment
Do not hesitate to call emergency services. This is if you or someone you know experiences these symptoms.
Regular Review and Updates
Your diabetes emergency plan is not a static document. It should be reviewed and updated regularly. This should be done at least every six months. Review it after any changes in your medication or health status. Make sure to update the plan. This plan must reflect any new information. Keep your emergency contacts informed of any updates.
Living Well with Diabetes
Living with diabetes requires proactive management. It also needs careful preparation. A comprehensive diabetes emergency plan is a key component. It helps you stay safe and healthy. By understanding the risks, recognizing the symptoms, and creating a plan, you can be prepared. You will be ready for anything. You can live a full and active life. Remember to consult with your healthcare provider. They can help you create a plan. This plan will meet your specific needs. [See also: Diet and Exercise Tips for Diabetics]
This article provides essential information. It is not a substitute for professional medical advice. Always consult with your healthcare provider for personalized guidance. Early preparation and awareness are crucial. This will improve your health and well-being. It will also improve your quality of life. Managing diabetes is a journey. Be prepared and stay informed.