Diabet Sleep Plan: Optimizing Overnight Control for People with Diabetes
Living with diabetes presents numerous challenges, and one of the most significant is managing blood sugar levels throughout the day and night. The overnight period, in particular, can be a critical time, as hormonal fluctuations and other factors can lead to unpredictable blood glucose readings. This article delves into the importance of a Diabet Sleep Plan, offering strategies and insights to help individuals with diabetes achieve better overnight control, ultimately improving their overall health and well-being.
The Critical Link Between Sleep and Diabetes
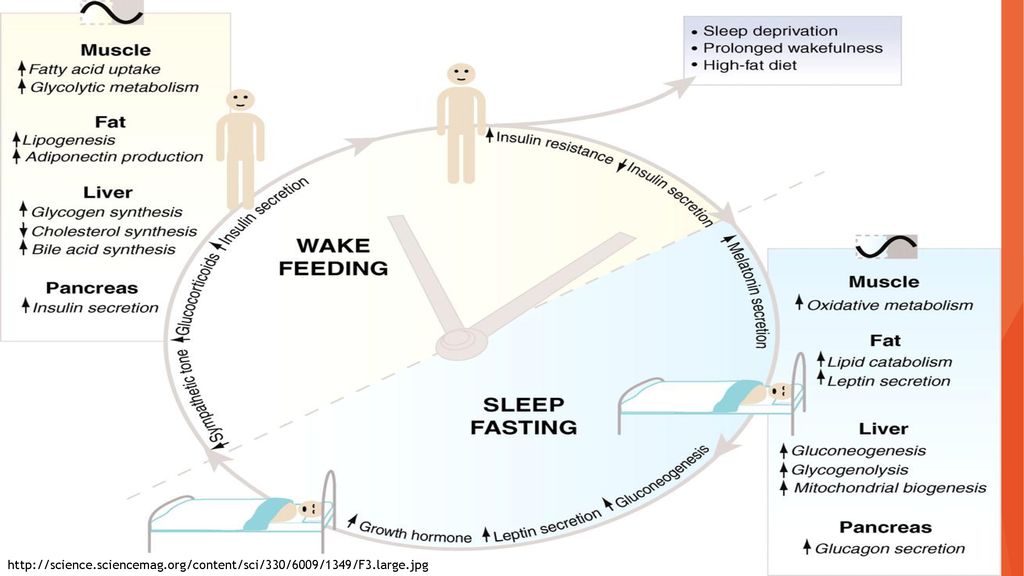
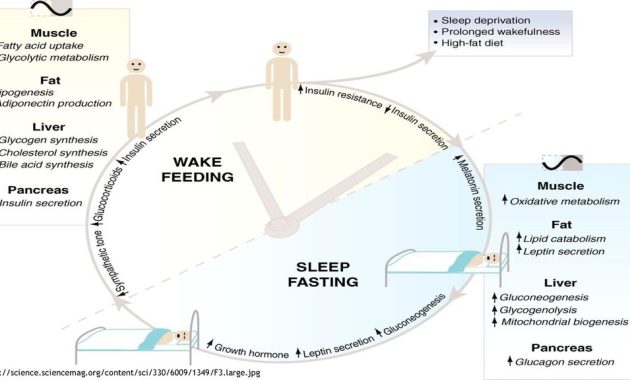
The relationship between sleep and diabetes is complex and bidirectional. Poor sleep quality and insufficient sleep duration are strongly associated with increased insulin resistance and impaired glucose metabolism. This means the body becomes less efficient at using insulin, leading to higher blood sugar levels. Conversely, uncontrolled blood sugar can also disrupt sleep, creating a vicious cycle.
Several physiological mechanisms explain this connection. During sleep, the body releases hormones that regulate blood sugar, such as cortisol and growth hormone. When sleep is disrupted, these hormonal processes are thrown off balance, leading to increased blood sugar levels. Moreover, sleep deprivation can trigger the release of stress hormones, such as cortisol, which further elevates blood sugar.
Understanding Overnight Blood Sugar Fluctuations
Many people with diabetes experience blood sugar fluctuations during the night. Several factors can contribute to this:
- Dawn Phenomenon: This is a natural surge in blood sugar that occurs between 4 a.m. and 8 a.m. as the body prepares to wake up. The liver releases glucose, and insulin resistance increases.
- Somogyi Effect: This occurs when blood sugar drops too low during the night (hypoglycemia), triggering the release of counterregulatory hormones that cause a rebound high blood sugar (hyperglycemia) in the morning.
- Insulin Dosing: The type and timing of insulin doses, especially long-acting insulin, can significantly impact overnight blood sugar levels.
- Dietary Choices: The carbohydrate content of the evening meal and bedtime snacks can influence blood sugar overnight.
- Other Health Conditions: Conditions such as sleep apnea can also affect blood sugar control.
Crafting a Personalized Diabet Sleep Plan
Creating a successful Diabet Sleep Plan requires a personalized approach. It’s essential to work closely with a healthcare provider, including a doctor, certified diabetes educator, and potentially a sleep specialist, to develop a plan tailored to individual needs and circumstances. The plan should address several key areas:
Optimizing Sleep Hygiene
Good sleep hygiene is the foundation of any effective Diabet Sleep Plan. This involves establishing healthy sleep habits to promote restful sleep:
- Consistent Sleep Schedule: Go to bed and wake up at the same time every day, even on weekends, to regulate the body’s natural sleep-wake cycle.
- Relaxing Bedtime Routine: Develop a relaxing pre-sleep routine, such as taking a warm bath, reading a book, or listening to calming music.
- Create a Sleep-Conducive Environment: Ensure the bedroom is dark, quiet, and cool. Use blackout curtains, earplugs, or a white noise machine if needed.
- Limit Screen Time Before Bed: Avoid using electronic devices (phones, tablets, computers) for at least an hour before bed, as the blue light emitted from these devices can interfere with sleep.
- Avoid Caffeine and Alcohol Before Bed: These substances can disrupt sleep patterns.
- Regular Physical Activity: Engaging in regular physical activity can improve sleep quality, but avoid strenuous exercise close to bedtime.
Dietary Considerations for Overnight Control
Diet plays a crucial role in managing blood sugar overnight. The evening meal and bedtime snacks should be carefully planned to prevent blood sugar fluctuations:
- Balanced Evening Meal: The evening meal should include a balance of carbohydrates, protein, and healthy fats.
- Portion Control: Avoid overeating at dinner, as this can lead to higher blood sugar levels.
- Bedtime Snack (If Needed): If necessary, a small bedtime snack can help prevent hypoglycemia. Choose a snack that combines carbohydrates and protein, such as a small apple with peanut butter or a few whole-grain crackers with cheese.
- Carb Counting: Learn how to count carbohydrates and adjust insulin doses accordingly, especially for the evening meal and bedtime snacks.
- Consult a Registered Dietitian: A registered dietitian specializing in diabetes can provide personalized dietary recommendations.
Insulin Management Strategies
Proper insulin management is essential for controlling blood sugar overnight. This involves working with a healthcare provider to:
- Determine the Right Insulin Regimen: The type and dosage of insulin will depend on individual needs and the type of diabetes.
- Adjust Insulin Doses: Insulin doses may need to be adjusted based on blood sugar readings and other factors, such as exercise and diet.
- Consider Insulin Pump Therapy: For some individuals, an insulin pump can provide more precise insulin delivery and better overnight blood sugar control.
- Learn to Use Continuous Glucose Monitoring (CGM): CGM devices continuously monitor blood sugar levels, providing valuable data to identify trends and make informed decisions about insulin doses and other adjustments.
- Understand Insulin Action Times: Know how long each type of insulin lasts.
Monitoring and Adjustments
Regular blood sugar monitoring is critical for evaluating the effectiveness of a Diabet Sleep Plan and making necessary adjustments. This should include:
- Checking Blood Sugar Regularly: Monitor blood sugar before bed, during the night (if needed), and upon waking.
- Using a CGM: CGM devices can provide a more complete picture of blood sugar patterns throughout the night.
- Keeping a Blood Sugar Log: Record blood sugar readings, insulin doses, food intake, and any other relevant information.
- Reviewing Data with Healthcare Provider: Regularly review blood sugar data with a healthcare provider to identify patterns and make adjustments to the Diabet Sleep Plan.
- Addressing Hypoglycemia and Hyperglycemia: Learn how to recognize and treat both low and high blood sugar.
Addressing Underlying Medical Conditions
Certain medical conditions can affect blood sugar control and sleep. Addressing these conditions is an important part of the Diabet Sleep Plan:
- Sleep Apnea: Sleep apnea, a condition where breathing repeatedly stops and starts during sleep, is common in people with diabetes and can worsen blood sugar control. Treatment for sleep apnea, such as CPAP therapy, can significantly improve both sleep and blood sugar levels.
- Depression and Anxiety: These mental health conditions can disrupt sleep and affect blood sugar. Addressing depression and anxiety with therapy and/or medication can improve both sleep and diabetes management.
- Other Medical Conditions: Other conditions, such as thyroid disorders and hormonal imbalances, can also affect blood sugar and sleep.
Potential Challenges and Solutions
Implementing a Diabet Sleep Plan can present challenges. Here are some common issues and potential solutions:
- Dawn Phenomenon: If experiencing dawn phenomenon, discuss with your doctor about adjusting insulin doses or considering a bedtime snack.
- Somogyi Effect: Monitor blood sugar during the night and consider adjusting insulin doses or eating a bedtime snack.
- Inconsistent Sleep Schedule: Strive for a consistent sleep schedule.
- Difficulty Adhering to Dietary Recommendations: Work with a registered dietitian to create a meal plan that is both healthy and enjoyable.
- Emotional Challenges: Diabetes can be emotionally challenging. Seek support from a therapist, support group, or diabetes educator.
The Benefits of Better Overnight Control
Improving overnight blood sugar control offers numerous benefits for people with diabetes, including:
- Reduced Risk of Complications: Better blood sugar control reduces the risk of long-term diabetes complications, such as heart disease, kidney disease, nerve damage, and eye problems.
- Improved Energy Levels: Stable blood sugar levels lead to more consistent energy levels throughout the day.
- Better Sleep Quality: Improved blood sugar control can lead to better sleep quality.
- Enhanced Mood and Cognitive Function: Stable blood sugar can improve mood and cognitive function.
- Overall Improved Quality of Life: Effective diabetes management leads to a better overall quality of life.
Seeking Professional Guidance
Creating and implementing a Diabet Sleep Plan is a collaborative effort that requires the expertise of healthcare professionals. It is highly recommended to consult with the following:
- Your Primary Care Physician: Your doctor can provide an overview of your overall health and help coordinate your care.
- A Certified Diabetes Educator (CDE): A CDE can provide education and support on diabetes management, including insulin therapy, diet, and exercise.
- An Endocrinologist: An endocrinologist specializes in hormone-related disorders, including diabetes, and can help manage complex cases.
- A Registered Dietitian: A registered dietitian can provide personalized dietary recommendations.
- A Sleep Specialist: A sleep specialist can help diagnose and treat sleep disorders.
By working closely with healthcare professionals and following a comprehensive Diabet Sleep Plan, individuals with diabetes can significantly improve their overnight blood sugar control and enhance their overall health and well-being. This proactive approach can lead to a healthier, more fulfilling life.
[See also: Related Article Titles]